Exploratory trial of a biepitopic CAR T-targeting B cell maturation antigen in relapsed/refractory multiple myeloma
multiple myeloma, 多发性骨髓瘤, chimeric antigen receptor modified T cells,经修饰的嵌合抗原受体 T 细胞, biepitope,双核, BCMA, cytokine release syndrome,细胞因子释放综合征 LabEX支持文献- Proc Natl Acad Sci U S A
- 2019
- 11.1
- 2019 May 7;116(19):9543-9551.
- human
- luminex
- serum
- 免疫/内分泌
- 骨髓癌
Abstract
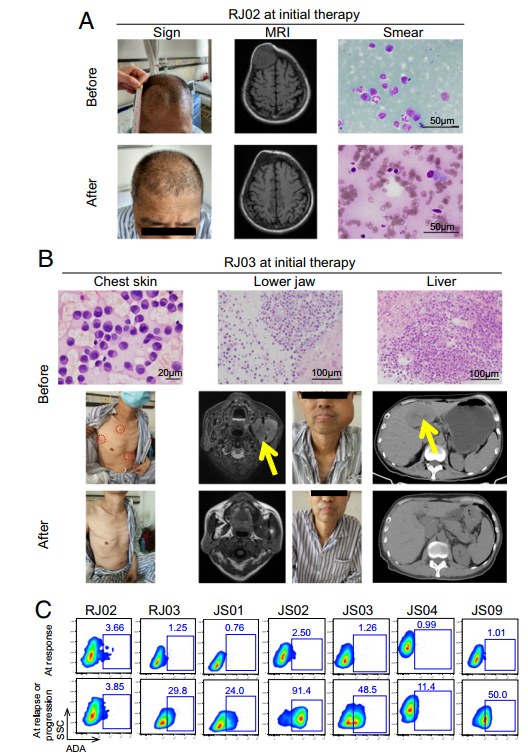
Relapsed and refractory (R/R) multiple myeloma (MM) patients have very poor prognosis. Chimeric antigen receptor modified T (CAR T) cells is an emerging approach in treating hematopoietic malignancies. Here we conducted the clinical trial of a biepitope-targeting CAR T against B cell maturation antigen (BCMA) (LCAR-B38M) in 17 R/R MM cases. CAR T cells were i.v. infused after lymphodepleting chemotherapy. Two delivery methods, three infusions versus one infusion of the total CAR T dose, were tested in, respectively, 8 and 9 cases. No response differences were noted among the two delivery subgroups. Together, after CAR T cell infusion, 10 cases experienced a mild cytokine release syndrome (CRS), 6 had severe but manageable CRS, and 1 died of a very severe toxic reaction. The abundance of BCMA and cytogenetic marker del(17p) and the elevation of IL-6 were the key indicators for severe CRS. Among 17 cases, the overall response rate was 88.2%, with 13 achieving stringent complete response (sCR) and 2 reaching very good partial response (VGPR), while 1 was a nonresponder. With a median follow-up of 417 days, 8 patients remained in sCR or VGPR, whereas 6 relapsed after sCR and 1 had progressive disease (PD) after VGPR. CAR T cells were high in most cases with stable response but low in 6 out of 7 relapse/PD cases. Notably, positive anti-CAR antibody constituted a high-risk factor for relapse/PD, and patients who received prior autologous hematopoietic stem cell transplantation had more durable response. Thus, biepitopic CAR T against BCMA represents a promising therapy for R/R MM, while most adverse effects are clinically manageable.
聚焦CAR-T治疗多发性骨髓瘤,LabEx助力细胞治疗研究
多发性骨髓瘤(multiple myeloma)是一种恶性浆细胞病称为浆细胞骨髓瘤,主要特征为免疫球蛋白或轻链过度生成,常伴随多发性溶骨性损害、高钙血症、肾脏损害等。该疾病具有和差的预后,本研究对17例复发难治性多发性骨髓瘤患者采取针对B细胞成熟抗原的CAR-T治疗(LCAR-B38M)进行干预,结果提示生物表位CAR - T对抗BCMA代表了一个有前途的治疗R/R MM的方法,而大多数不良反应在临床上是可以控制的。
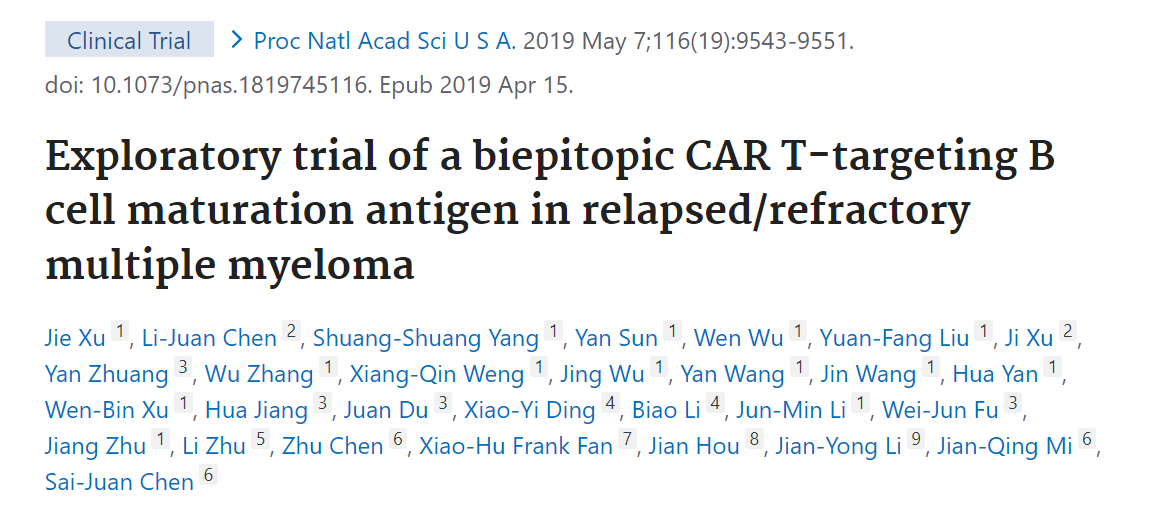
文章中CAR – T研究数据展示:17个参与患者的临床和血液指标情况。
患者静脉输注CAR-T细胞后,监测血液中细胞的数量发现CAR-T细胞在第二天开始上升,PCR和FACS也得到同样的结果,在绝大多数患者中CAR-T细胞持续存在,最高可达9个月之久。

LCAR-B38M的功效
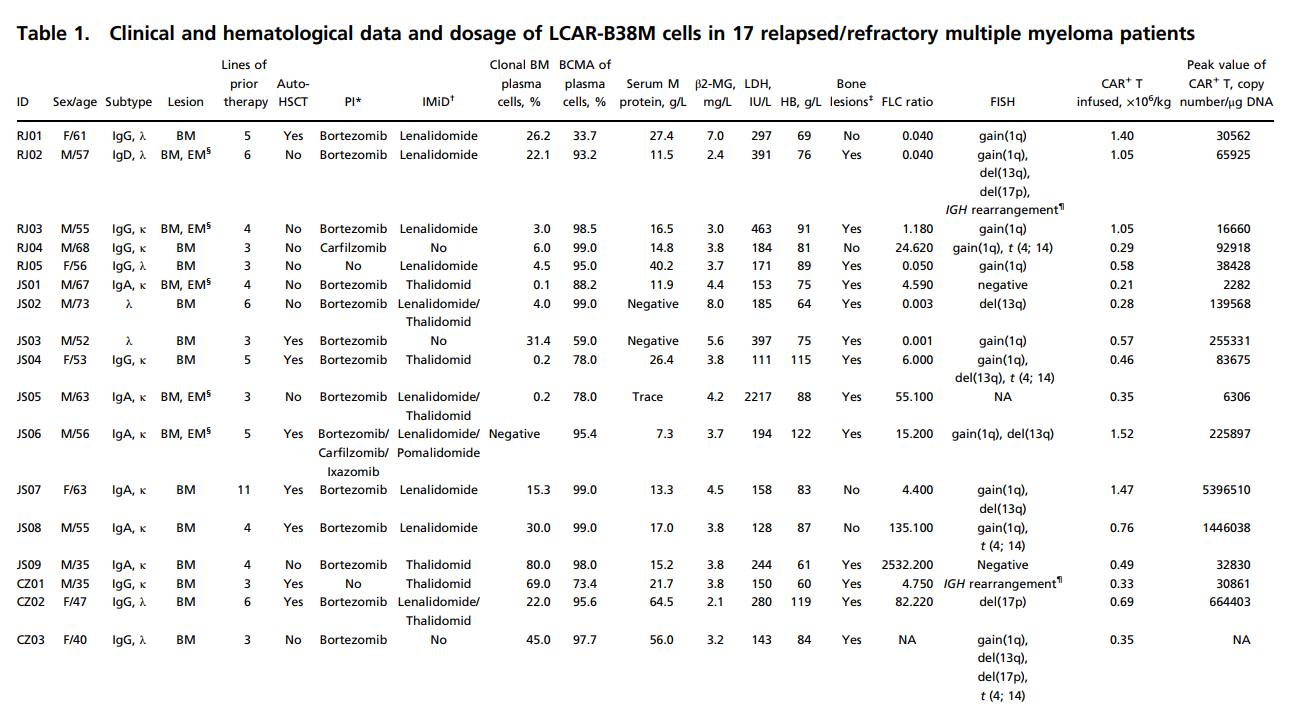
对17例患者的资料合并分析,在CAR - T治疗后1个月,15例患者获得了反应,1例无明显反应,另1例因严重的CRS/TLS而不幸早亡。在分析15例有反应患者的最大治疗效果时,13例达到了严格的完全缓解,2例达到了很好地部分缓解。在17例患者12至535天,8例(47.1%),包括7例sCR和1例VGPR,仍处于持续缓解状态,所有这些患者在CAR - t后持续缓解超过11个月,6例sCR后复发,1例VGPR后出现进展性疾病(PD),曲线显示无进展生存(PFS)率6个月时为 82.4%,12个月时52.9%。1年总生存率(OS)为82.3%。
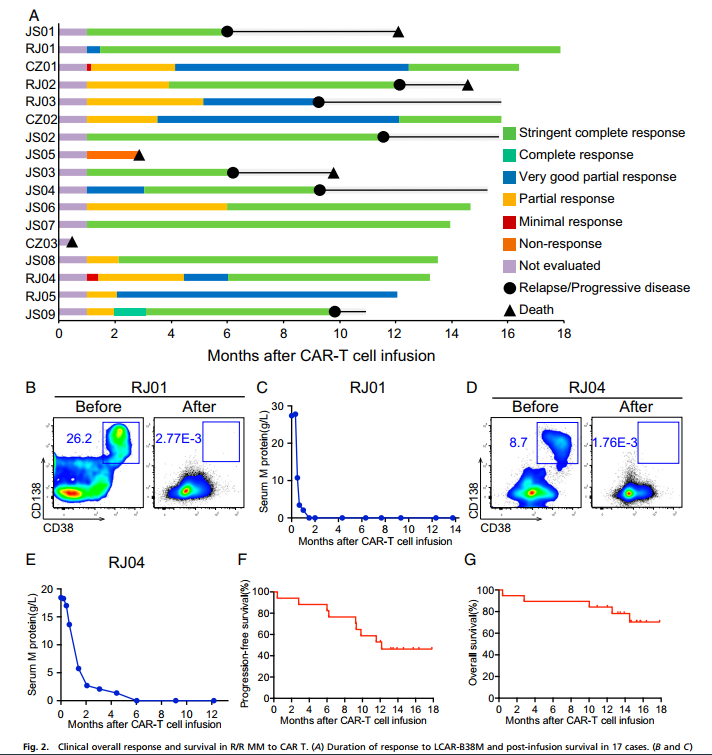
患者RJ02 CAR-T治疗4个月后,浆细胞瘤明显减少,原发部位未见占位性病变;RI03患者,CAR-T治疗后,第19天皮肤肿块消失,6个月后肝脏占位性病变消失;
不良影响及其管理
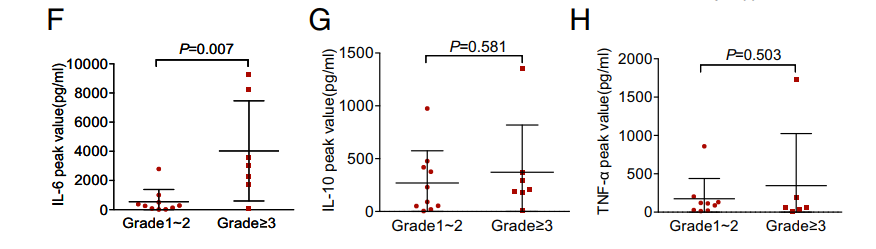
CAR-T治疗最常见的不良反应是细胞因子风暴,临床表现伴随显著上调的血清细胞因子谱。52.9%的患者出现1级以上肝功能障碍,主要表现为天门冬氨酸转氨酶升高。在LCAR-B38M治疗之后,我们通过luminex技术实时监测患者血清中IL-6, IL-10, and TNF-α的表达,发现三种细胞因子均有升高趋势,其中IL-6上升最高。
综上所述:针对B细胞成熟抗原的CAR-T治疗(LCAR-B38M),在多发行骨髓瘤中发挥着一定作用,伴随的细胞因子风暴等不良反应也能欧够被有效的控制,研究结果证明,三次输注和一次输注两种输注方式的亚组之间没有明显的疗效和毒性差异。
本网站销售的所有产品及服务均不得用于人类或动物之临床诊断或治疗,仅可用于工业或者科研等非医疗目的。







 沪公网安备31011502400759号
沪公网安备31011502400759号
 营业执照(三证合一)
营业执照(三证合一)


